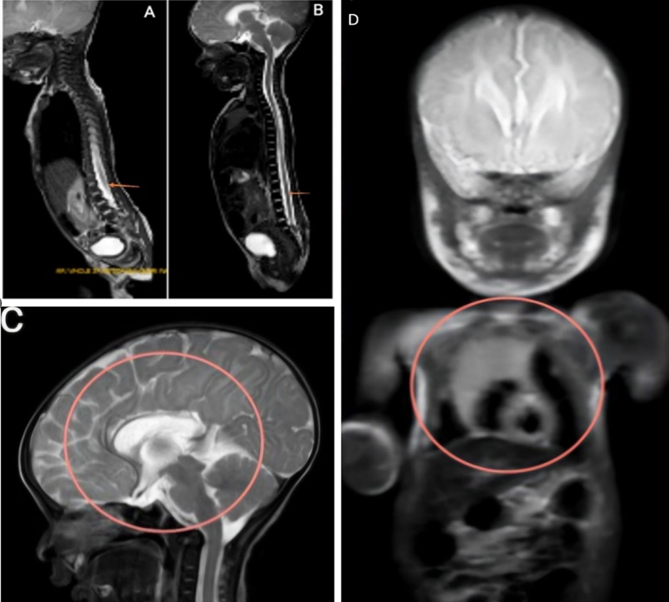
A rare and complex presentation of congenital anomalies: meningomyelocele, corpus callosum agenesis, and dextrocardia in a neonate
Sakshi Desai, Sharath Hullumani
PAMJ. 2025; 52:136. Published 03 Dec 2025 | doi:10.11604/pamj.2025.52.136.46847
Corresponding author
Sharath Hullumani, Department of Paediatrics Physiotherapy, Ravi Nair Physiotherapy College, Datta Meghe Institute of Higher Education and Research (DU), Sawangi (Meghe), Wardha, India (sharathhullumani@gmail.com)
This image
| Articles published in PAMJ are Open Access and distributed under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0). |  |

eISSN: 1937-8688
The Pan African Medical Journal (ISSN: 1937-8688) is a subsidiary of the Pan African Medical Journal. The contents of this journal is intended exclusively for professionals in the medical, paramedical and public health and other health sectors.
Currently tracked by: DOAJ, AIM, Google Scholar, AJOL, EBSCO, Scopus, Embase, IC, HINARI, Global Health, PubMed Central, PubMed/Medline, ESCI
Physical address: "Kenya: 3rd Floor, Park Suite Building, Parkland Road, Nairobi. PoBox 38583-00100, tel: +254 (0)20-520-4356 | Cameroon: Immeuble TechnoPark Essos, Yaounde, PoBox: 10020 Yaounde, tel: +237 (0)24-309-5880"





