Factors associated with acceptability of HIV self-testing (HIVST) among university students in a Peri-Urban area of the Democratic Republic of Congo (DRC)
Ben Bepouka Izizag, Hippolyte Situakibanza, Tathy Mbutiwi, Richard Ingwe, Florian Kiazayawoko, Aliocha Nkodila, Madone Mandina, Murielle Longokolo, Evelyne Amaela, Marcel Mbula
Corresponding author: Ben Bepouka Izizag, Division of Infectious Diseases, University Teaching Hospital of Kinshasa, Kinshasa, Democratic Republic of Congo 
Received: 10 Sep 2017 - Accepted: 07 Dec 2018 - Published: 27 Dec 2018
Domain: Public health
Keywords: Acceptability, HIV self-test, students
©Ben Bepouka Izizag et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Ben Bepouka Izizag et al. Factors associated with acceptability of HIV self-testing (HIVST) among university students in a Peri-Urban area of the Democratic Republic of Congo (DRC). Pan African Medical Journal. 2018;31:248. [doi: 10.11604/pamj.2018.31.248.13855]
Available online at: https://www.panafrican-med-journal.com//content/article/31/248/full
Original article 
Factors associated with acceptability of HIV self-testing (HIVST) among university students in a Peri-Urban area of the Democratic Republic of Congo (DRC)
Factors associated with acceptability of HIV self-testing (HIVST) among university students in a Peri-Urban area of the Democratic Republic of Congo (DRC)
Ben Bepouka Izizag1,&, Hippolyte Situakibanza1, Tathy Mbutiwi2, Richard Ingwe3, Florian Kiazayawoko4, Aliocha Nkodila1, Madone Mandina1, Murielle Longokolo1, Evelyne Amaela1, Marcel Mbula1
1Division of Infectious Diseases, University Teaching Hospital of Kinshasa, Kinshasa, Democratic Republic of Congo, 2Faculty of Medicine, University of Kikwit, Kinshasa, Democratic Republic of Congo, 3National Program of HIV/AIDS and STD, Kinshasa, Democratic Republic of Congo, 4Division of Internal Medicine, Hospital of Boma, Kinshasa, Democratic Republic of Congo
&Corresponding author
Ben Bepouka Izizag, Division of Infectious Diseases, University Teaching Hospital
of Kinshasa, Kinshasa, Democratic Republic of Congo
Introduction: this paper examines the acceptability of HIV self-testing (HIVST) by students in a university in the DRC and identifies factors associated with uptake of HIVST.
Methods: a cross-sectional study was conducted with a sample of 290 students from Kikwit University. Data were summarized using proportions and predictions of acceptability of HIVST by logistic regression.
Results: the average age of students was 22.5 years, with the majority of the students being male (57%). Just over half the students sampled, reported being sexually active (51.8%). One hundred and sixty four (75%) reported that they had one sexual partner and fifty-six (25%) two or more sexual partners in the past year. Sixty-six percent had used condoms during their last sexual encounter. The acceptability of HIVST was high (81.4%) and 66.1% of students stated that they would confirm the self-test at a local health facility. The knowledge about the importance of the self-test (OR 5.02; 95% CI:1.33-18.88; p=0.017), the perception that counseling pre and post-test were important (OR 2.91; 95% CI:1.63-5.19; p < 0.0001) and the willingness to realize the test with a partner (OR 2.46; 95% CI:1.43-4.23; p=0.034) were factors associated with HIVST.
Conclusion: the acceptability of HIVST was high and therefore its implementation is feasible in our country. However, prior to implementation, additional factors such as cost; access of HIVST; false reassurance of the test; missed early infections in the window period, limited counseling and linkage to care options, need to be considered.
In recent years, there has been increasing optimism around achieving an AIDS-free generation [1]. The Joint United Nations Program on HIV/AIDS has outlined its ambition for supporting such an AIDS-free generation, by establishing a series of goals to this end. These goals can be summarized as the UN HIV 90-90-90 program. This program aims to ensure that 90% of people living with HIV/AIDS (PLWHA) know their status, to initiate 90% of these individuals on treatment and to achieve a viral load suppression in 90% of this group [2]. Reaching these targets will require bolstering the entire cascade of HIV care, which in turn, starts with getting more people tested for HIV [3, 4]. In an effort to achieve the United Nations (UN) 90-90-90 global HIV target and specifically the first target of diagnosing of 90% of all people with HIV, the World Health Organization (WHO) released the consolidated guidelines on HIV testing services in 2015. Therein, they highlighted the potential of HIV self-testing (HIVST) to increase HIV testing service (HTS) access, especially among men, key populations and young people. They also highlighted the need to improve the uptake of couples and partner testing services, including offering HTS to the partners of people with HIV [5]. Young people, aged between 15 and 24, are particularly vulnerable to both acquiring and transmitting HIV and more than 50% of all new infections worldwide are among young people between within this age group [6]. The HIV test was developed in mid-1980 and was intended to be accompanied with HIV counseling [7]. However, with the growing awareness of HIV/AIDS and the recent availability of antiretroviral therapy (ART), the scope and reasons for voluntary counseling and testing (VCT) have broadened. These services are essential components of HIV prevention and care programs. In the past many people were reluctant to be tested even if the care program and treatment were available to them [8]. Thus, HIVST has the potential to facilitate the testing of more people, because it has advantages of convenience, speed, privacy and accessibility, thus eradicating many of the barriers that prevent people from being tested. It also has the potential to be an acceptable option for high risk populations who would not otherwise be tested using currently available HIV counseling and testing (HCT) services for various reasons [9]. The adoption and implementation of HIVST as a testing option in many African countries as well as globally does however come with challenges. Health experts and government stakeholders have criticized the technology for its risk of inaccurate results, potential psychological risk posed by a lack of adequate counseling and uncertainty over unsupervised linkage to care for individuals who test positive for HIV [10-12]. Here we have conducted a study to assess the implementation of HIVST intervention among young people in the DRC. The objective of this study was to evaluate the acceptability of HIVST and identify factors associated with HIVST among students in Kikwit University.
Study area and study period: this study was conducted from March to April 2017 in Kikwit University.
Study design: cross sectional study design.
Study population: all current students of Kikwit University were considered as the study population.
Study setting and sample: an institution based cross sectional study was conducted in Kikwit University, which was founded in 1992 and is located in Kikwit city in the Kwilu Province, a peri-urban area 500 KM from Kinshasa, in the South-west of the Democratic Republic of Congo. It is one of the prestigious public institutions. The university has four departments (faculties) which are medicine, law, agronomy and economics with a total of 2525 students enrolled.
Sampling: the sample size was computed by using the following formula:
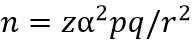
where p represents the proportion of acceptability to HIVST, taking the proportion of 87.1% [13] and considering a 10% non-response rate, q (1 - p) and z, the value of the standard normal distribution corresponding to a significance level of alpha of 0.05 (1.96). We assumed, d (the precision degree) to be 5%. Using the equation we calculated a minimal sample size of 208 students. A total of 290 students were selected by using a stratified sampling technique and the number of study participants for each selected department was obtained from the registrar's office. The total sample size was allocated proportionally according to the size of all four selected faculties and then simple random sampling was employed to select students from each faculty. The students were asked to fill out the questionnaire at their leisure.
Exclusion criteria: students who studied in the eve evening were excluded from the study.
Instrument of data collection and techniques: data was collected by using a self-administered structured questionnaire which was printed in French. The study's instruments were the self-administered and structured questionnaire that included questions on socio-demographic background, sexual behavior, HCT practices and opinions and the acceptability of HIVST. We used a validated questionnaire from the Australian and South African Students and Sexual Health Survey [13, 14]. During our study, Students were asked about whether they would use HIVST, their willingness to buy self-testing kits, their opinions on the provision of the pre- and post-testing for HIVST and also about the information on how to use self-testing kits. For evaluating the acceptability and opinions of the students about HIVST, we asked students if they were aware of HIVST, whether they would like to start using HIVST as a testing option, whether pre and post-test counseling was necessary for HIVST, and also if they were willing to buy a self-test kit. We also asked them if they would encourage their partner to do the HIVST and if they would submit the test results for statistical purposes. Additionally we asked if they would confirm a positive test result by going to a local clinic. All test results, whether positive or negative have been submitted for collating with the HCT statistics.
Data collection and quality control: data collection was conducted by four general practitioners. Data collectors received a half day training in using the questionnaires (topics included: the objective of the study, how to approach the participants, how to administer and collect the questionnaires on the time). Consequently, the questionnaire was revised, taking into account the advice of the practitioners, before data collectors were disseminated to collect data. Confidentiality of the study participants was maintained during distribution and data collection periods. Above all, ethics, coding and entry were maintained throughout the process.
Data analysis: prior to data entry, the questionnaires were checked for completeness. Partially completed questionnaires were excluded from analysis. The questionnaires were coded and the data entered into Excel and analyzed by the SPSS Version 21 package. Collected data was summarized with the use of frequency, percentage and odds ratios. Binary/multiple logistic regression analyses were used in order to assess the association and measure the level of significance. Further logistic regression was used to adjust for possible confounding factors and the results were reported by using P < 0.05 level of statistical significance.
Ethical considerations: ethical approval was obtained from the Ethics committee of the University of Kinshasa. Consent was requested and obtained from each student prior the study. No personal identification was recorded on the questionnaire for ethical reason.
Demographics, sexual behaviors and the HCT opinions of the students: of the two hundred ninety students who participated in this study, 57% were male and 43% female. The average age of the students was 22 years (age range 19±33 years). Most of the students (n = 154.63) were between 20 and 24 years old. Half of the students (51.8%) reported regular sexual activity. 74.5% reported having only one partner, 16.4% two partners and 9.1 % more than two partners. 52% of students reported the use of condoms when having sex. A total of 46.9% of the participants had never been tested for HIV, while 39.9% of students reported that they knew the HIV status of their sexual partner/s. The majority of the participants, 95.5%, considered HIV testing to be important for young people and 92.5% said that HIV pre-test counseling was necessary (Table 1).
Opinions and acceptability regarding HIVST: in the present study, 54.5% of the participants were aware of HIVST before the survey. The acceptability of HIVST as a testing option was 81.4%. The proportion of students who indicated the necessity for pre-test counseling for HIVST was 70.4%. Seventy three percent of students agreed on the necessity for post-testing kit counseling for the HIVST and 78. 4% expressed a willingness to buy self-testing kits themselves. Sixty eight point four percent of students agreed to use HIVST with their partners. We also found that 55.5 % were willing to submit the HIVST results to a local clinic for inclusion in the HCT statistics. The target of the HCT uptake campaign was 55.5%. The willingness to confirm a HIV positive self-test result at a local health care facility was 66.1% (Table 2).
Factors associated with the uptake of HIVST: in order to determine factors associated with uptake of HIVST among students in the University of Kikwit, multivariate logistic regression analyses were performed. Independent variables included demographic (age and gender), sexual behavior (sexual relationships, number of sexual partners and use of condoms), HCT practices and opinions of the students (having been tested for HIV before, knowledge of HIV status of their sexual partners, knowledge of the importance of the HIV test, the necessity of HIV pre-test counseling, the willingness to submit HIVST results at a local clinic for inclusion in the HCT statistics, to confirm HIV positive self-test results at a local health care facility, the willingness to buy a HIVST and to share' an HIVST with their partner). These factors were compared against the outcome variables in a multivariate linear regression model. The acceptability of HIVST in this model, the knowledge of the importance of the test (OR : 5.02 95% CI:1.33-18.88, p=0.017), and perception of counseling the pre and post-test are important (OR : 2.91 95% CI : 1.63-5.19, p < 0.0001) were calculated. The willingness to realize the test with a partner (OR: 2.46 95% CI:1. 43-4. 23, p=0.034) was another factor associated with HIVST (Table 3).
According to the consensus statement from the first international symposium on HIVST, despite a lack of data regarding its effect on populations, HIVST has a vast potential to scale-up access to HTC services [15]. However, before promoting it widely, the WHO/UNAIDS meeting highlighted the need for evidence-based studies on the potential implementation of HIVST programs in various settings. Our study is a contribution towards this goal by providing data on acceptability of HIVST as well as the demographic and behavioral factors that are associated with the uptake of HIVST among students in the DRC. This study assessed the students' HIV testing practices, using the available HCT services, the acceptability of HIV self-testing and other associated factors among students in Kikwit University before the implementation of this strategy in the DRC. Half the students in this study had had a sexual relationship and 33.3% of these reported having multiple sexual partners. Forty eight percent did not use a condom in their last sexual encounter. This result matches findings of Mogkatle et al in South Africa. Contrary to Mogkatle's results, half of the students in the Kikwit sample knew their serologic status. This result was lower than the finding of Mogkatle et al (72%). This may be explained by the difference between a Southern African versus Central African setting and the fact that Kikwit is a peri-urban site while the South African study was conducted in an urban site [13]. Our data suggests that there is a high frequency (81.4%) of acceptability of HIV testing among students of Kikwit and 68% of them would take up HIV self-testing with their respective partners. The high HIVST acceptability has also been illustrated in different population groups in other studies in Sub-Saharan countries [13, 16-18]. It is possible that with the roll-out of a HIVST program, the frequency of HIV testing among students could therefore increase. At the international symposium on HIVST [15], a concern was raised that the frequency of HIVST alone should not be used as a preventive strategy. The WHO has highlighted the importance of the message that HIVST does not provide a verified diagnosis on HIV, but requires further testing. Therefore despite its ease of use and high acceptability, illustrated in this study, HIVST should contain clear instructions for the use and interpretation of results, as well as how to access the HIV prevention, care and treatment services [19]. Based on the models assumptions, we realize that the lower titers of antibodies and the longer window period of the available oral HIVST kit have more false negative results than facility-based HTC [20]. In terms of confirming positive test results, more than half of the students (66 %) reported their intention to confirm their HIV positive self-test at a local health care facility. This result was lower than that found by Mogkatle et al in South Africa (75%) and higher than that found by Kurth et al in Kenya (35.5%) [13, 21]. In South Africa, the awareness raised about HIV infection is higher than the DRC. It has been recommended that self-testing be in some way linked to a health care facility so that diagnosis can be associated with confirmation and treatment. However currently, there are no reported examples of referral mechanisms to link people who self-test to treatment and care [10].
Van Royen.H and his colleagues [8] suggested that the self-testing instruction kits should provide adequate information on what to do after self-testing. In our study we did not include any questions regarding instructions in the test kit. It is possible that if interviewers had explained that the kit would instruct a person on what do after testing that less than 34% of the students would have reported no intention to confirm their self-test results. It is important that the provision of HIVST, as with all HTC services, includes programming and messaging about how to access and link a patient to HIV prevention, care and treatment services. There is no doubt that the pre- and post-test counseling remains a challenge for the scaling up of HIVST. The accessibility of services must complement the convenience of HIVST. This could be achieved by toll-free hotlines for example. This will be vital for the scaling up and implementation of HIVST. A number of factors which were associated with the uptake of HIVST among these students, such as: the knowledge of the importance of the test, their perception of pre and post-test counseling and the willingness to take the test with a partner are recognised as important indicators of HIV awareness and prevention. Regarding the knowledge of the importance of the test, HIV counseling and testing (HCT) are among the most effective and important interventions for managing the HIV epidemic [22]. There is substantial evidence showing the link between increased HCT and reduced HIV incidence [23, 24]. One of the problems of existing HCT programs leading to a lack of knowledge of HCT is that leaners are only counseled once they make the decision to test. By including HCT, the pre-test counseling can take place sooner within a general health setting before a decision to test is taken. The increase in knowledge and confidence in the HCT process is likely to act as an individual facilitator. In reality, while counseling is offered to everybody who undergoes HCT, counselors may have different levels of training, and have different attitudes towards clients [25]. Their perception that counseling pre and post-test is important, is itseld a critical factor. This was the second factor associated to acceptability of HIVST in our study. In the case of adolescents, counseling has a wider value; as it is a phase of life in which new skills and abilities are acquired which con¬tribute to ensuring self-care in health throughout adulthood. The diagnosis of a chronic and incurable disease like AIDS in adolescence has a greater impact, since it may cause several changes in the daily life, in the student life and in the process of socialization outside the family environment [26]. From the psychological point of view, adolescence coincides with the first realization of loss and grief [27]. When an adolescent has a serious illness in this period, these losses and grief will be much more painful and difficult to overcome, and the experience of the disease can bring greater suffering. In this sense, the man¬ner in which the pre- and post-HIV test counseling is executed is of vital importance and can increase or reduce the impact of diagnosis and treatment [28]. The third associated factor was the willingness to take the test with a partner. HIV self-testing is a novel strategy that is attractive to both women and men and may prove better at reaching male partners than many other current methods. By its very nature, HIVST is more flexible and autonomous than other forms of HTC and therefore may provide an alternative avenue to the narrow definitions of couples-HTC. Gender and power relations will continue to shape the different stages of decision making, but the ability to discretely determine the circumstances and timing upon which a test is take has been shown to be empowering. This may enable women to influence domestic decision-making without provoking negative reactions from their male partners [29].
Most of the students in this study freely accepted HIVST and agreed to encourage their partner to do the test as well. The knowledge of the importance of the test, perception of counseling the pre and post-test and the willingness to take the test with their partner were factors associated with HIVST. The results suggest that the implementation of the test is feasible in our country, but still premature because of concerns such as the cost, access of HIVST, the possibility of false negative test results and missed early infections in the key window period. Additionally limited counseling and linkage to care options are factors that will also need to be addressed, should this strategy be implemented.
Limitations: the limitations of this study are that we cannot assume causality of the statistically significant associations with acceptability of HIVST in this study given its cross-sectional design. It is possible that unknown or unmeasured factors could have confounded the estimates of the observed associations in our results. The data show a high proportion of willingness to use HIVST but a low linkage to care after self -testing. Some questionnaires were not answered in full, which lead to missing data points; however the sample size in the analysis was adjusted to account for this problem.
What is known about this topic
- HIV self-testing (HIVST) is globally accepted as an important complement to existing HIV counseling and testing (HCT) approaches;
- The acceptability of HIVST among students and the population groups with poor uptake of HCT remain limited in Africa;
- HIVST can be performed accurately and it is an acceptable and feasible testing approach in a variety of contexts; including populations at ongoing HIV risk and those who may not otherwise be tested.
What this study adds
- Half of students interviewed were sexually active but the use of condom was not high despite a high desire to use the HIVST;
- A majority of students had the will to confirm the result of a HIVST in a local health care facility, which reinforces the link between the patients and the health system;
- The implementation of the HIVST is not possible now in our country taking into account issues related to accessibility and false belief of a negative result within the window period.
The authors declare no competing of interests.
Ben Bepouka Izizag participated in proposal writing, data collection, analysis, interpretation and critical review of the manuscript. Hippolyte Situakibanza, Tathy Mbutiwi, Richard Ingwe participated in proposal writing, data analysis, interpretation and critical review of the manuscript. Murielle Longokolo, Madone Mandina and Evelyne Amaela participated in data analysis, interpretation and critical review of the manuscript. Marcel Mbula participated in data analysis, interpretation and critical review of the manuscript. They also read and approved the final manuscript.
We acknowledge all students of Kikwit University who accepted to participate in this study. We thank Linda Mikado for English translate.
Table 1: demographics, sexual behaviors and the HCT opinions of the students
Table 2: opinions and acceptability regarding HIVST
Table 3: factors associated with the uptake of HIVST
- Fauci AS, Folkers GK. Towards an AIDS-free generation. JAMA. 2012 July 25; 308(4): 343-4. PubMed | Google Scholar
- UNAIDS. 90-90-90: an ambitious treatment target to help and end the AIDS epidemic. In. Edited by Joint United Nations Program on HIV/AIDS (UNAIDS). 2014. Accessed May 12 2017.
- Abdool Karim SS. Overcoming impediments to global implementation of early antiretroviral therapy. N Engl J Med. 2015 Aug 27; 373(9): 875-6. PubMed | Google Scholar
- McMahon JH, Medland N. 90-90-90: how do we get there. The Lancet HIV. 2014; 1(1): e10-1. PubMed | Google Scholar
- WHO. Consolidated guidelines on HIV testing services. Geneva: World Health Organization; 2015. Accessed May 11 2016.
- Tan X, Pan J, Zhou D, Wang C, Xie C. HIV/AIDS knowledge, attitudes and behaviors assessment of Chinese student: a questionnaire study. Int J Environ Res Public Health. 2007; 4(3): 248-53. PubMed | Google Scholar
- Shangula MN. Factors affecting voluntary counseling and HIV testing among pregnant women in Tsumeb district, Oshikoto region, Namibia. Community Health Department, Western Cape University. 2006. Google Scholar
- Van Rooyen H, Tulloch O, Mukoma W, Makusha T, Chepuka L, Knight LC et al. What are the constraints and opportunities for HIVST scale-up in Africa: evidence from Kenya, Malawi and South Africa. JIAS. 2015 Mar 20; 18: 19445. PubMed | Google Scholar
- Gardner J. HIV home testing-a problem or part of the solution. South African Journal of Bioethics and Law. 2012; 5(1): 15-19. Google Scholar
- Makusha T, Knight L, Taegtmeyer M, Tulloch O, Davids A, Lim J et al. HIV Self-Testing Could" Revolutionize Testing in South Africa, but It Has Got to Be Done Properly": Perceptions of Key Stakeholders. PloS one. 2015; 10(3): e0122783. PubMed | Google Scholar
- Mavedzenge SN, Baggaley R, Corbett EL. A review of self-testing for HIV: research and policy priorities in a new era of HIV prevention. Clin infect Dis. 2013 jul; 57(1): 126-38. PubMed | Google Scholar
- Myers JE, El-Sadr WM, Zerbe A, Branson BM. Rapid HIV self-testing: long in coming but opportunities beckon. AIDS. 2013 Jul 17; 27(11): 1687-95. PubMed | Google Scholar
- Mokgatle MM, Madiba S. High acceptability of HIV Self-Testing among Technical Vocational Education and Training College Students in Gauteng and North West Province: what are the implications for the scale up in South Africa?. PLoS ONE. 2017 Jan 31; 12(1): e0169765. PubMed | Google Scholar
- Smith A, Agius P, Mitchell A, Barrett C, Pitts M. Secondary students and sexual health 2008, Monograph Series No 70, Melbourne. Australian Research Centre in Sex, Health & Society, La Trobe University. 2009.
- World Health Organization. Report on the first international symposium on self-testing for HIV. Geneva: 2013. Accessed 27 May 2017.
- Gaydos CA et al. The uptake and accuracy of oral kits for HIV self-testing in high HIV prevalence setting: a cross-sectional feasibility study in Blantyre, Malawi. PLoS Med. 2011; 8(10): e1001102. PubMed | Google Scholar
- Kumwenda M, Munthali A, Phiri M, Mwale D, Gutteberg T, MacPherson E et al. Factors shaping initial decision-making to self-test amongst cohabiting couples in urban Blantyre, Malawi. AIDS Behav. 2014 jul; 18(4): 396-404. PubMed | Google Scholar
- Kalibala S, Tun W, Cherutich P, Nganga A, Oweya E, Oluoch P. Factors associated with acceptability of HIV self-testing among health care workers in Kenya. AIDS Behav. 2014 jul; 18(4): S405-14. PubMed | Google Scholar
- Kalibala S, Tun W, Muraah W, Cherutich P, Oweya E, Oluoch P. 'Knowing myself first': feasibility of self-testing among health workers in Kenya'. Nairobi: population council. 2011. Google Scholar
- Katz DA, Cassels SL, Stekler JD. Replacing clinic-based tests with home-use tests may increase HIV prevalence among Seattle men who have sex with men: evidence from a mathematical model. Sex Transm Dis. 2014; 41(1): 2-9. PubMed | Google Scholar
- Kurth AE, Cleland CM, Chhun N, Sidle J, Were E, Naanyu V et al. Accuracy and acceptability of oral fluid HIV Self-Testing in a general adult population in Kenya. AIDS Behav. 2016; 20(4): 870-879. PubMed | Google Scholar
- Schwartländer B, Stover J, Hallett T, Atun R, Avila C, Gouws E et al. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet. 2011 Jun 11; 377(9782): 2031-41. PubMed | Google Scholar
- Coates TJ, Kulich M, Celentano DD, Zelaya CE, Chariyalertsak S, Chingono A et al. Effect of community-based voluntary counselling and testing on HIV incidence and social and behavioural outcomes (NIMH Project Accept; HPTN 043): a cluster-randomised trial. Lancet Glob Heal. 2014 May; 2(5): e267-77. PubMed | Google Scholar
- Rosenberg NE, Westreich D, Bärnighausen T, Miller WC, Behets F, Maman S et al. Assessing the effect of HIV counselling and testing on HIV acquisition among South African youth. AIDS. 2013; 27(17): 2765-73. PubMed | Google Scholar
- MIET Africa. Literature Review: Youth friendly health services. 2011.
- Vieira MA, Lima, RAG. Children and adolescents with chronic disease: living with changes. Rev Latino-Am Enfermagem. 2002; 10(4): 552-560. PubMed | Google Scholar
- Aberastury A, Knobel M. Adolescência normal. Porto Alegre: Artes Médicas. 1998.
- Taquette SR, Adriana OR, Bortolotti LR. Perception of pre-and post-HIV test counseling among patients diagnosed with aids in adolescence HIV test counseling for adolescent. Cienca saude coletiva. 2017; 22(1):23-30. PubMed | Google Scholar
- Kumwenda M, Munthali A, Phiri M, Mwale D, Gutteberg T. Factors shaping initial decision-making to self-test amongst cohabiting couples in Urban Blantyre, Malawi. AIDS Behav. 2014; 18: S396-S404. PubMed | Google Scholar











